For several years, I was Executive Director of a charity that provided prescription medicines to people who couldn’t afford them. I saw remarkable examples of medicines improving people’s lives. One patient had severe asthma and was going to the emergency room repeatedly because he couldn’t breathe. We provided him with medicine and his attacks stopped. The improvement in his life was remarkable.
Stories like this are not uncommon. Many of us know someone whose cancer was cured because of medical innovation. We now have a cure for Hepatitis C. There are remarkable treatments for rheumatoid arthritis and many other chronic illnesses.
The power of medical innovation to make lives better has created controversy about the costs of new prescription medicines. Understandably, those who suffer from illness want access to medicines that can cure or manage those illnesses.
While running the charity, I would occasionally run into someone claiming that we needed to put price caps on the cost of medicines. They would point to the price in other countries with government-run healthcare as an example of what could happen. The reality, though, is that price caps would harm the very innovation that makes innovative treatments so attractive in the first place. It is a great example of killing the goose laying the golden eggs.
Despite that reality, President Trump recently signed an executive order intended to arbitrarily limit the price of prescription medicines. This is a bad idea for several reasons. First, such critical and impactful polices should not be adopted by the stroke of a pen by the president, who has no legislative authority. If Congress wants prices controls then they should have the courage to adopt them.
The policy itself, however, would make life worse for millions of people in the United States, now and in the future. Having worked first-hand to deliver medicines to patients in-need, I know there is a better approach that helps people get treatments and encourages innovation.
There are many reasons innovative prescription medicines are expensive. First is that it is simply difficult to treat complex diseases. Finding treatments that target illness without side effects is extremely challenging. It takes time and resources, and there are many dead ends.
Our regulatory processes don’t make it any easier. Much of the drug development process is designed around satisfying government regulations. Approval by government agencies can be somewhat arbitrary. One of the most famous examples is the story of John Nestor, who worked at the FDA and became famous for refusing to approve new medicines. Basing access to new medicines on the judgment of one man in government is a bad idea.
Given those realities, innovation in health care is costly. Much of the low-hanging fruit has been picked.
Some will still say it is not fair that other countries pay less than we do for the same drug. “Fairness” has been the justification for many foolish government policies. Washington state’s recent rent control legislation was specifically justified based on the argument that it strikes a “fair balance.” Of course, that is completely subjective and depends on the whims of politicians. Risking the housing market or medical innovation based on what politicians think is fair is a dangerous path.
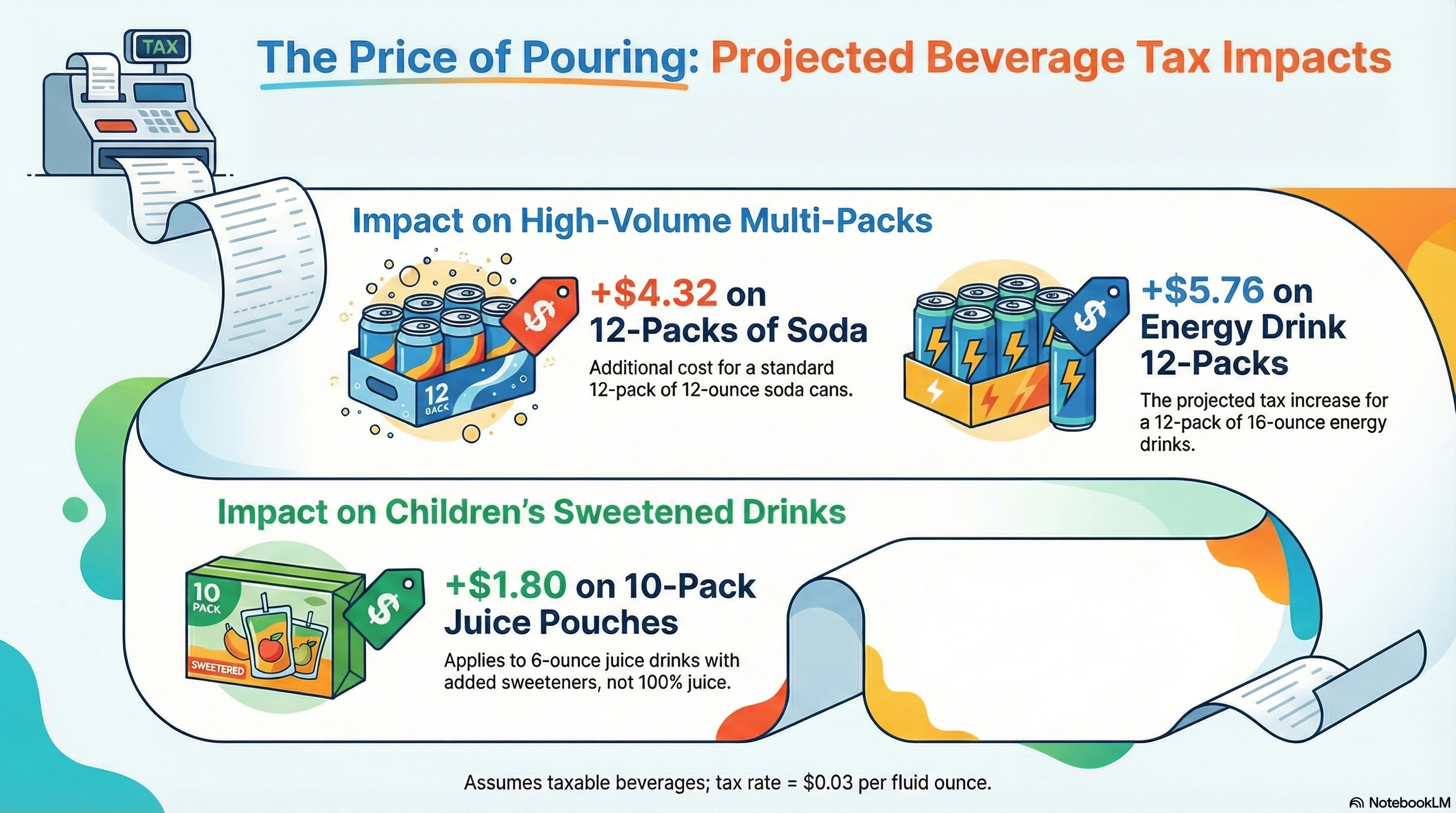
The reason Americans pay more for some medicines is that other countries have legally mandated price caps. Those caps are above the marginal price of producing the medicines, so drug companies are willing to sell to those countries. They understand that those sales don’t pay for the cost of the innovation but do provide a small profit. Of course, if the companies could charge more and spread the costs of developing new drugs across more countries and consumers, they would. But given half a loaf or nothing, they understandably choose half a loaf.
If the US now imports price-controls from other countries with government-run healthcare systems, access to existing medicines and future innovation would be put at risk. We would be cutting off our nose to spite our face.
It would mean that there would be fewer new medicines to treat difficult illnesses.
Government programs like Medicaid and health insurers already cut costs by switching patients to older, generic medicines rather than new medicines. Medicaid referred many people to my charity because state government restricts what medicines are available and when a doctor specifically requested a newer medicine, government programs frequently refused to provide it. The justification for rationing access is the same as for the executive order – trying to cut prices. The need for those treatments didn’t go away. The patients just had to look for alternatives. Fortunately, we helped some of those people.
And while generics can be a good alternative, that isn’t always the case. When a new mental health drug was released, we received a huge number of requests for help for that medicine. Previous mental health drugs had serious side effects and were more like sedation than treatment. Although the newer medicine was more expensive, it allowed people to control their mental illness and live a more normal life. Switching people to generics can cut costs, but it is not a panacea.
How, then do we provide incentives to innovate in that difficult environment while reaching as many people as possible with new medicines?
The best answer is a hybrid of allowing drug companies to charge prices that allow them to recover the costs of innovation plus profit, encourage competition that puts downward pressure on prices and providing charity support to those who cannot afford them. There will still be gaps. I saw many of them first-hand. But it is far better than a one-size-fits-all policy imposed by the federal government that rations care.
Some countries will still pay less for medicines than the United States. The U.S. will still have some of the best healthcare in the world and access to medical innovations that helped the patients I worked with. An approach that encourages innovation while caring for those in need strikes the best balance between affordability and creating treatments that help people live longer and healthier lives.