Key Findings
1. The United States spends more money on health care than any other country. Advocates of a single-payer health care system argue that the U.S. has worse outcomes than other industrialized countries, in spite of the high cost.
2. The two organizations that are most often cited on international health care rankings are the World Health Organization and the Commonwealth Fund. Both groups penalize the U.S. because the country does not have government-mandated universal health insurance.
3. Simply having health insurance does not guarantee timely access to medical care.
4. Research shows that the U.S. ranks either first or in the top five countries when dealing with the two most common health issues – cardiovascular disease and cancer.
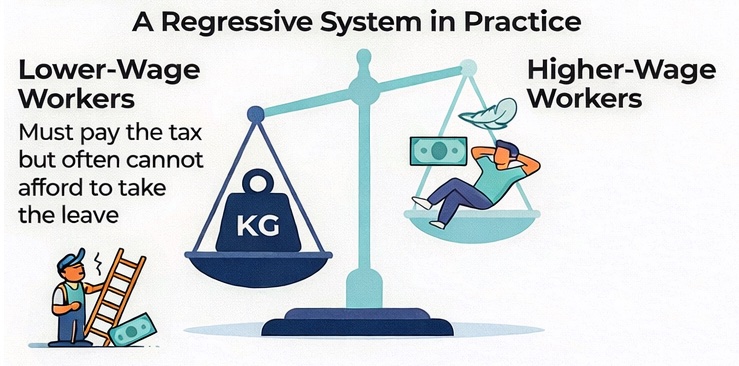
5. Personal responsibility is critically important to maintaining good health but is virtually always overlooked when discussing health care delivery systems.
6. A country’s health care system cannot and should not be responsible for individual lifestyle choices, which in many cases contribute to illness. The effectiveness of health care delivery should be based on clinical outcomes.
Introduction
The United States spends more money on health care than any other country. In 2019, the year before the COVID-19 pandemic, the U.S. spent $3.8 trillion, or 17.7 percent of the economy’s gross domestic product (GDP), on medical care. The question is whether this amount of spending provides better clinical outcomes for patients.
Advocates of a socialist, single-payer health care system argue that the U.S. has worse health outcomes than other industrialized countries, all of which have some form of government-run medical care. At the same time, there is an increasing trend in the U.S. for payers, employers and government programs, to only reimburse providers for “quality” medicine.
This Policy Brief reviews data that compares clinical health outcomes in the U.S. with those of other countries. It examines how the criteria of “pay-for-quality” (PFQ) are generated and whether so-called PFQ policies provide any real benefit to patients. This study explores how data on “unnecessary” hospital deaths is collected. It also correlates the lifestyle choices of individuals with health outcomes.
Read the full Policy Brief here.