Biosimilar drugs offer the very real possibility of providing patients with quality alternative medicines and enhanced treatments at better prices. But bringing biosimilar drugs to patients depends on achieving a transparent, predictable, competitive marketplace, protected by strong intellectual property and regulatory systems.
Key Findings
- Biosimilar drugs and biobetter drugs offer the very real possibility of quality alternatives and even enhanced treatments at better prices.
- A policy of forcing the use of “cheaper” medicines has a chilling effect on patient care, medical innovation and economic investment.
- A clear understanding of science is essential to effective government regulation of biologic drugs.
- Biologic drugs are created from living organisms and are not as easy to replicate as traditional drugs like aspirin.
- The traditional regulatory approval pathway used for generic drugs will not work with biologic medicines.
- It is estimated that in a few years, innovative biologic medicines will comprise almost one-half of the top 100 best-selling drugs.
- Sustainable innovation must be protected to ensure the 21st century truly earns the title of the biomedical century.
First Do No Harm
It is often said that “sometimes a bargain is just too expensive.”
Physicians live in a world where cost concerns of patients, insurance companies and the government chaff against the freedom to practice the art and science of patient-centered care.
At the same time, legislators are constantly bombarded with public policy schemes that claim to solve the problem of providing more health care dollars at a time of historic belt cinching. To paraphrase H.L. Mencken, for every complex problem there is a simple solution — and it is usually wrong.
These are the tensions that exist in the world of health care reform and biosimilar medicines.
Here are some typical claims that generally accompany any discussion of biosimilar drugs:
“Savings from biosimilar drugs will cover the cost Medicaid expansion.”
“Biosimilar are the same thing as generic drugs.”
“Biosimilar drugs must achieve the same high FDA standards for approval.”
“Doctors want to switch patients from brand-name drugs to biosimilar copies.”
All these broad statements are incorrect. As common misconceptions they cause problems in examination rooms and legislative chambers nationwide because they prevent people from having a clear understanding of what biosimilar drugs are and how they impact patient treatment.
A policy of forcing the use of “cheaper” medicines also has a chilling effect on medical innovation and economic investment.
Wanting something to be true (whether a “magic pill” for a state’s budgetary woes or a “risk-free” way to reduce a patient’s medical expenses) should not cloud the judgment of lawmakers or physicians. Careful consideration of the advantages and disadvantages of biosimilar drugs should be the guiding principle for both physicians and legislators to ensure we “first do no harm.”
This paper is a primer on biosimilar drug policy for both policymakers and physicians. As such, there are some terms and concepts that may be familiar to one group but not to the other, but in general this study seeks to avoid scientific and regulatory jargon.
Policymakers must seek out the counsel of physicians, medical and disease organization and, yes, also patient groups as they consider ways to address and implement health care reform. Biosimilars are but the most recent addition to that complicated and highly political conversation. When it comes to biosimilars, partisanship must be put aside because a legislative misstep based on a misunderstanding of the science (or the blinders of party loyalties) could have significant unintended consequences not just for budgetary reform, but for patient health and safety.
Biologics Defined Biologic medicines are large (5,000 to 20,000 atoms), complex molecules produced from living cells. Minor differences in manufacturing processes, such as different host cells, cell culture and purification methods, can have a clinically significant impact on a biologic drug’s safety and effectiveness. Biologic drugs will comprise an estimated 48% of the top 100 best-selling drugs by 2016. Unlike small molecule medications made from chemical processes, biologic drugs are made by using a living organism or its product as the starting point, which typically produces larger molecules such as proteins or enzymes. Biosimilar drugs are structurally highly similar versions of marketed biological medicines that are shown by appropriate analytical testing and clinical trials to to be sufficiently similar, both structurally and clinically, to to an original innovator biologic drug. Because biologic medicines are highly complex they require a wide variety of analytical methods to ensure consistent quality and patient safety. Given the complexity of biologic drugs and their manufacture, in which living cells are used to produce the core molecule, the innovator product has inherent lot-to-lot variability. In light of this inherent variability and the diverse and complex analytical methods required to identify the molecules, it is not realistic to replicate an innovator molecule exactly. Therefore, the development of a generic biologic drug is to make a molecule that is as similar to the innovator molecule as possible. Accordingly, generic molecules in the biologic industry are called biosimilar, rather than biogeneric. Biobetter drugs have the same target or mechanism of action as innovator biologic drugs, but they include structural changes that may result in better efficacy at treating disease or fewer drug-related side effects. |
Cost versus Care in the Age of Personalized Medicine
The age of the blockbuster prescription drug is over. Cost concerns are more challenging than ever. And we are struggling with what “personalized medicine” really means.
Today we are in in the era of post-patent medicine where advances in manufacturing and molecular diagnostics are as important as discovering new molecular entities and drug safety is as important and difficult to prove as efficacy.
This is also a time of biologic biosimilar medicines. But will biosimilars really be as important an element of change as many believe? Will they be a game changer?
Will all the changes that biosimilars bring positively affect the advancement of public health? Many people believe the expectations that biosimilars will radically reduce costs are overstated. Others fear that safety concerns are being understated and that the risks to innovation are real.
What Is a Biologic Medicine?
The term “biologic” is used to classify medicines derived from living sources. They can be used for diagnosis, prevention and therapeutics. Unlike traditional drugs that are chemically synthesized, biologics are developed from a biologic process. Biologic manufacturing is extremely complex. Consequently, it is insufficient to define the product by just its molecular composition. Instead, a product is also defined by the process through which it is made.
Biologics are typically composed of large molecules, whereas traditional chemical drugs are made up of small molecules.
The Process Is the Product
A clear understanding of science is essential to effective government regulation of biologic drugs.
Understanding the process that creates the drug is at least as important as the product itself, if not more so. Minor differences in manufacturing processes, such as different host cells, cell culture and purification methods, can have a clinically significant impact on a biologic drug’s safety and effectiveness. This idea is summed up in the phrase “The process is the product.”
Biologic drugs have unique structural organization patterns (referred to as folding) that affect the way these function in the body. Even biologic drugs that visually appear the same may have differing biological effects due to differences in their structural folding.
An example of this folding effect is shown by the difference between a raw egg and a cooked one: chemically the two are the same, but physically and biologically they are very different.
What Is a Biosimilar Drug?
Biosimilar drugs (sometimes called follow-on biologics) are structurally similar versions of marketed biological medicines that are supported by appropriate analytical testing and clinical trials to demonstrate that they are sufficiently similar (both architecturally and clinically) to their reference innovator biologic drug. An innovator biologic drug is the original marketed medicine.
Biosimilar drugs are gaining attention because they supposedly reduce health care costs. However, even minor differences in manufacturing processes, such as different host cells, cell culture and purification methods, can have a clinically significant impact on both the safety and effectiveness of biologic drugs. Many people fear the Food and Drug Administration’s (FDA) truncated regulatory requirements for approving biologic drugs trade off faster review for less real-world data on safety and efficacy.
Any discussion of biosimilar drugs and their safety must first recognize that there is no such thing as a “generic” biologic drug. Biologic drugs are created from living organisms and are not as easy to replicate as traditional drugs like aspirin and antihistamines.
To establish that two biologic medicines are similar and can be safely substituted for one another, the sponsor of a follow-on product would need to demonstrate through clinical trials that repeated switching from the original biologic drug to the substitute biosimilar drug (and vice versa) provides effective treatment of disease and does no harm to patients.
Biosimilars are usually authorized on the basis of abbreviated FDA applications, demonstrating they are the same in structure as, and bioequivalent to, a previously authorized product. Non-clinical and clinical data are not usually required. Although the generic drug approval process has been in place in much of the world for several decades, it has been generally recognized for some time that the same approval process will not work for biologically derived drugs.
Sameness, Medical Efficacy and Patient Safety
The traditional regulatory approval pathway used for generic drugs will not work with biologic medicines because of the complexity of both the molecules and the manufacturing processes. Biosimilar drug safety is not the same as generic drug safety.
When it comes to biosimilars, the most important issues facing global drug regulators are the scientific and technical factors related to a determination of biosimilarity or interchangeability.
As with “small molecule” generic medicines, “large molecule” biosimilar drugs will be considered by some as interchangeable with their innovator antecedents — and, just like generic medicines, there is a significant potential that repeated switching between similar biologic products will have a negative impact on patient safety and clinical effectiveness.
Government regulators must determine when a biosimilar drug is interchangeable with its reference product.
The scientific oversight for the development of original biologic drugs is time tested and well understood. However, across the globe, government regulators are struggling to develop new rules for the approval and oversight of biosimilar drugs. Since biosimilar drugs are never exact copies of the original medicine, establishing appropriate standards for clinical development, manufacturing processes and therapeutic use remains an unsettled and important area of regulatory debate.
Government regulators must develop policies to guide if and when a pharmacist may automatically substitute a biosimilar drug for a “name-brand” biologic medicine prescribed by a doctor. In some cases, these policies may be evaluated in conjunction with government drug policies for drug reimbursement.
Biosimilar Drugs, Therapeutic Substitution and Health Care Reform
The issue of biosimilar drugs and therapeutic substitution will be at or near the top of the budget agenda in state capitols across the United States. Biosimilars are a medical option, but as every state in the union attempts to tighten its budget, requiring patients to use biosimilar drugs is an enticing, but incorrect and dangerous policy option. Placing short-term budgetary considerations before long-term patient well-being is pennywise and pound foolish, and is deleterious to both the public purse and public health.
This is an even more urgent policy issue since now, under the new federal health care reform law, The Patient Protection and Affordable Care Act, insurance policies sold to individuals and small businesses must cover 10 essential health benefits, including prescription drugs. State lawmakers will have to determine how insurance companies cover those benefits within their own borders.
Twenty-eight members of the U.S. House of Representatives have sent a letter to the U.S. Department of Health and Human Services (HHS) expressing concern about a Center for Medicare and Medicaid Services (CMS) proposal that may allow insurers to cover only one drug per therapeutic class. Such a requirement would be “overly restrictive,” they say. The letter correctly points out that the proposed CMS policy ignores patients’ clinical needs and would lead to poorer clinical outcomes and greater health care costs.
Scientific and Regulatory Challenges Reference Product – Against what innovative product(s) may a biosimilar be compared to support its authorization? Quality – What data must a biosimilar application include and what must be proved to show that a biosimilar’s quality is sufficiently comparable to that of the innovator product? Non-clinical Data – What type and amount of non-clinical data (including data comparing a biosimilar drug to its referenced innovator product) are needed? What data must be provided to support a drug’s “biosimilarity”? Clinical Trials – Under what circumstances is clinical data needed to support a biosimilar drug’s authorization? What type of data is needed (such as pharmacokinetic, pharmacodynamic, efficacy, safety or immunogenicity)? Extrapolation of Indications – Under what circumstances may a biosimilar receive authorization for a different clinical indication than the reference product? Naming – What proprietary and/or non-proprietary names should be permitted or required for biosimilar drugs? How will physicians select the specific drug to be dispensed? How will manufacturers and regulators distinguish the various biologics for pharmacovigilance purposes? Labeling – How will biosimilars be labeled (for example, what information from the reference product’s label may or must appear in the biosimilar’s labeling)? Must a biosimilar drug’s labeling indicate that the product is a biosimilar? Interchangeability and Substitution – What data must be provided to allow a regulatory authority to conclude that a biosimilar drug is interchangeable with its reference product? Will the biosimilar have the same clinical efficacy and side effects as the innovator biologic? Data Protection – What is a reasonable length of time for patent protection? What is a reasonable time period to allow innovator companies to recoup their research and development costs, as well as insure future biologic development? |
What about Adverse Events?
Regulatory authorities worldwide must address how to effectively trace adverse patient events (complications and bad patient outcomes) to the use of a specific biologic drugs or biosimilar products so that when problems arise they can be traced back to the appropriate cause. This will be complicated by the fact that different countries will have different biosimilar drug availability and different drug naming policies.
Many countries are developing policies that will allow a pharmacist to automatically substitute a biosimilar drug in place of the specific medicine prescribed by a physician without requiring the physician’s consent. Automatic therapeutic substitution not only undermines a physician’s ability to choose the best treatment for her patients, but also complicates the choice of drugs required to ensure patient safety.
Can We Ever Trade Cost for Care?
The friction between cost and patient care is rarely discussed by those who see biosimilar drugs exclusively as a cost-savings mechanism. But the blinders of cost-containment must never be permitted to obscure the twin therapeutic pillars of safety and efficacy.
In fact, when it comes to biosimilar drugs, the most important issues facing global drug regulators are the scientific and technical factors related to a determination of biosimilarity or interchangeability.
As an article in the Journal of Infection so aptly stated, “Nothing is more expensive than treatment failure.”
What about Cost?
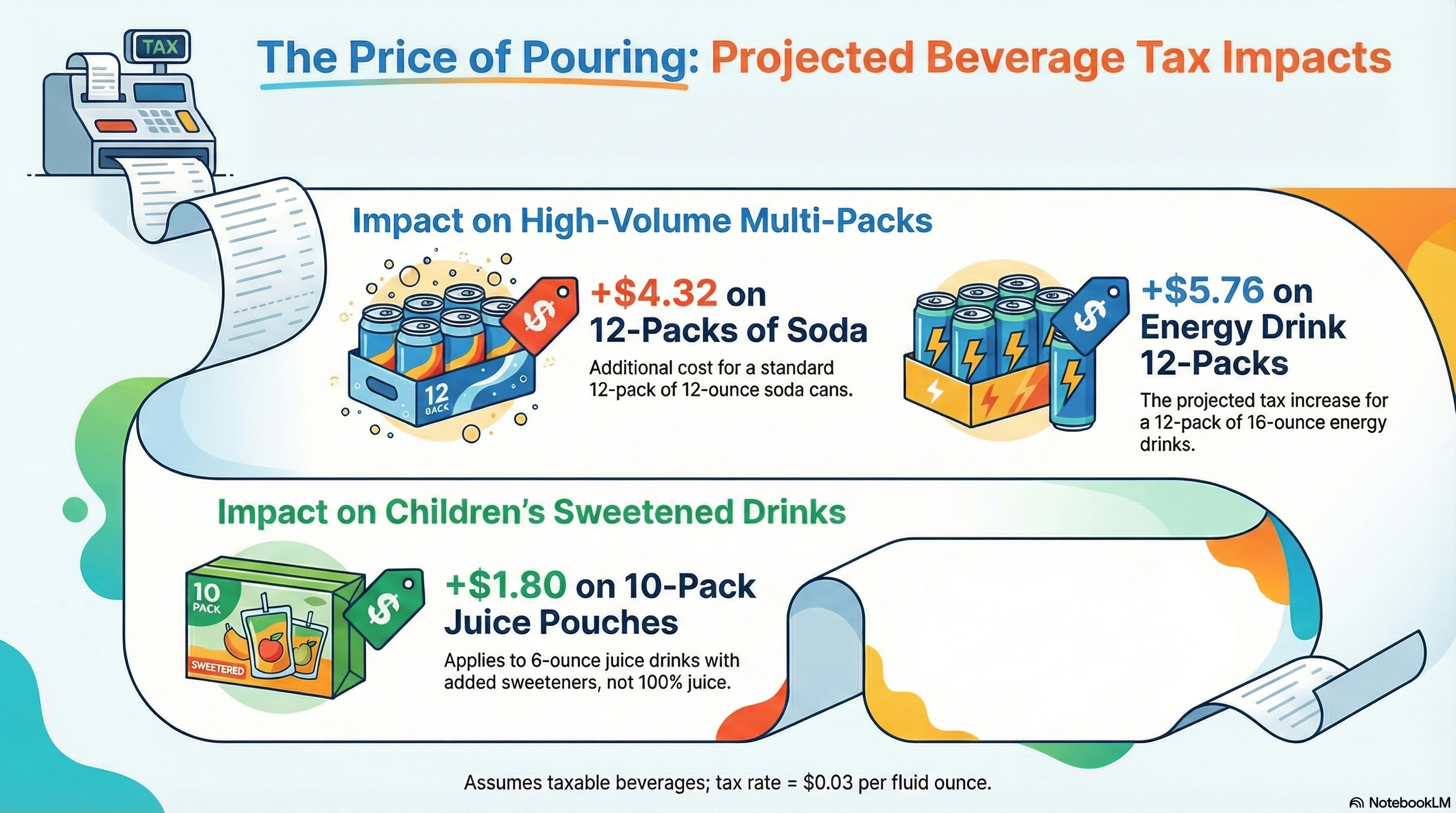
Another crucial difference between biosimilar drugs and traditional chemical generic drugs is that biosimilar drugs are difficult and expensive to get approved, complicated and challenging to manufacture, and have a short shelf life. The result is that the price difference between innovator biologic drugs and biosimilar drugs will be far narrower than the price between brand-name chemical drugs and their generic counterparts.
The likely modest cost difference between an innovator biologic drug and its biosimilar imitator will make it economically feasible for the innovator company to compete with its biosimilar competition. As a result, the cost savings to public programs from requiring patients to use biosimilar substitutes are likely to be much less than policymakers expect.
The European experience demonstrates that the market cost of a biosimilar drug is roughly 20% to 30% of the innovator price. So the question becomes, can innovator companies, once one of their medicines goes off patent, lower the prices of their brand name products and still make a profit? The answer is yes, and this provokes an important question for prescribers: Why would a physician prescribe an unfamiliar biosimilar drug (or a health care system prioritize a biosimilar for payment) when the original innovator drug is available at a competitive price?
The price of any medicine reflects its therapeutic value as well as the considerable costs and risks associated with investment in research and development. Today it takes about 10,000 new molecules in the lab to produce one FDA-approved medicine. And of these, only three out of 10 new medicines earn back their research and development costs. Unlike other research-intensive industries, pharmaceutical investments generally must be sustained for over two decades before the few successful medicines that make it to market can generate any profit.
But innovation is important, and not just for pharmaceutical industry profits. Increases in life expectancy resulting from better treatment of cardiovascular disease from 1970 to 1990 have been conservatively estimated as bringing benefits worth more than $500 billion a year. In 1974, cardiovascular disease was the cause of 39% of all deaths. Today it is about 25%. Cerebrovascular diseases were responsible for 11% of deaths back then. In 2004 they caused 6.3% of deaths. Kidney diseases were linked to 10.4% of deaths and now they are associated with 1.8%. And that’s just for the United States.
As Harvard University health economist (and President Obama health care advisor) David Cutler noted: “The average person aged 45 will live three years longer than he used to solely because medical care for cardiovascular disease has improved. Virtually every study of medical innovation suggests that changes in the nature of medical care over time are clearly worth the cost.”
A new discovery of an innovator biologic drug is the result of the complex, established and effective process that guides its development, manufacture and approval. Many health care systems are developing standards and practices to ensure that product quality and therapeutic value are not inappropriately eclipsed by short-term and transient cost considerations.
What Is a Biobetter Drug?
New, creative solutions can arise out of the complex and difficult drug research process. An excellent example of this is the development of biobetter drugs.
Biobetter drugs are to biosimilar drugs what Apple’s iPod Touch is to its iPod shuffle. Where a biosimilar drug will be a mere structural imitation, a biobetter drug possesses some molecular modification that constitutes an improvement over the original innovator drug.
Such improvements may range from a longer half-life, allowing for less frequent dosing, to more potency with less toxicity. That is innovation driven by the new reality of biosimilar competition. It shouldn’t be surprising since, among other things, competition drives innovation.
Biosimilar drugs and biobetter drugs offer the very real possibility of quality alternatives and even enhanced treatments at better prices. These scientific advances depend on a transparent, competitive marketplace, controlled by a predictable regulatory system.
Innovative Biologic Medicines Create Innovative Solutions for Patients
It is estimated that in a few years, innovative biologic medicines will comprise almost one-half of the top 100 best-selling drugs. Worldwide today, there are 168 innovator biologic medicines on the market helping a quarter of a billion people control or overcome disease, add years to their lives and improve their quality of life. But achieving scientific innovation is hard and success is never guaranteed.
Today, innovator drug companies are investing their time, talent and financial resources in developing new biologic medicines to treat more than 250 diseases. The incorrect use of biosimilar drugs puts the innovator companies, and more importantly patients who use the biosimilar drugs, at risk. Sustainable innovation must be protected to ensure the 21st century truly earns the title of the biomedical century.
Health care innovations must always place the patient at the center of the health care equation. The twin pillars of medical safety and efficacy must never be sacrificed to merely save costs, and physicians must always have a full array of therapeutic options at their disposal.
As the key issues highlighted in this paper are addressed by policymakers, regulators, physicians, payers and others, high-quality, safe and effective biosimilars will provide patients and prescribers additional treatment options and expand access by offering lower-cost alternatives for biologic medicines. The emphasis, however, must stay laser focused on “high-quality, safe and effective.”
About the Authors
Peter Pitts is president of the Center for Medicine in the Public Interest. A former member of the United States Senior Executive Service and former FDA Associate Commissioner, he supervised the FDA’s Office of Public Affairs, Office of the Ombudsman, Office of Special Health Issues, Office of Executive Secretariat and Advisory Committee Oversight and Management. He served on the agency’s obesity working group and counterfeit drug task force and is a Special Government Employee (SGE) consultant to the FDA’s Risk Communications Advisory Committee.
His comments and commentaries on health care policy issues regularly appear in media nationwide, including The New York Times, Los Angeles Times, The Washington Post, The Wall Street Journal, and Financial Times. He is the editor of Coincidence or Crisis, a discussion of global prescription medicine counterfeiting and Physician Disempowerment: A Transatlantic Malaise. A graduate of McGill University, Pitts has served as an adjunct professor at Indiana University and Butler University.
Dr. Roger Stark is a health care policy analyst at Washington Policy Center. He is the author of the book The Patient-Centered Solution: Our Health Care Crisis, How It Happened, and How We Can Fix It. He is also the author of numerous studies on state and national health care policy. Dr. Stark graduated from the University of Nebraska College of Medicine and completed his general surgery residency in Seattle and his cardiothoracic residency at the University of Utah. After practicing in Tacoma he moved to Bellevue and was one of the co-founders of the open heart surgery program at Overlake Hospital. He retired from private practice in 2001 and became actively involved in the hospital’s foundation, serving as Board Chair and Executive Director. Dr. Stark has been a member of many local and national professional societies. He is a past member of the Governing Board of Overlake Hospital, currently serves on the Board of the Washington Liability Reform Coalition, and is an active member of the Woodinville Rotary.
Download a PDF of this Policy Brief here.